MAKE A DONATION
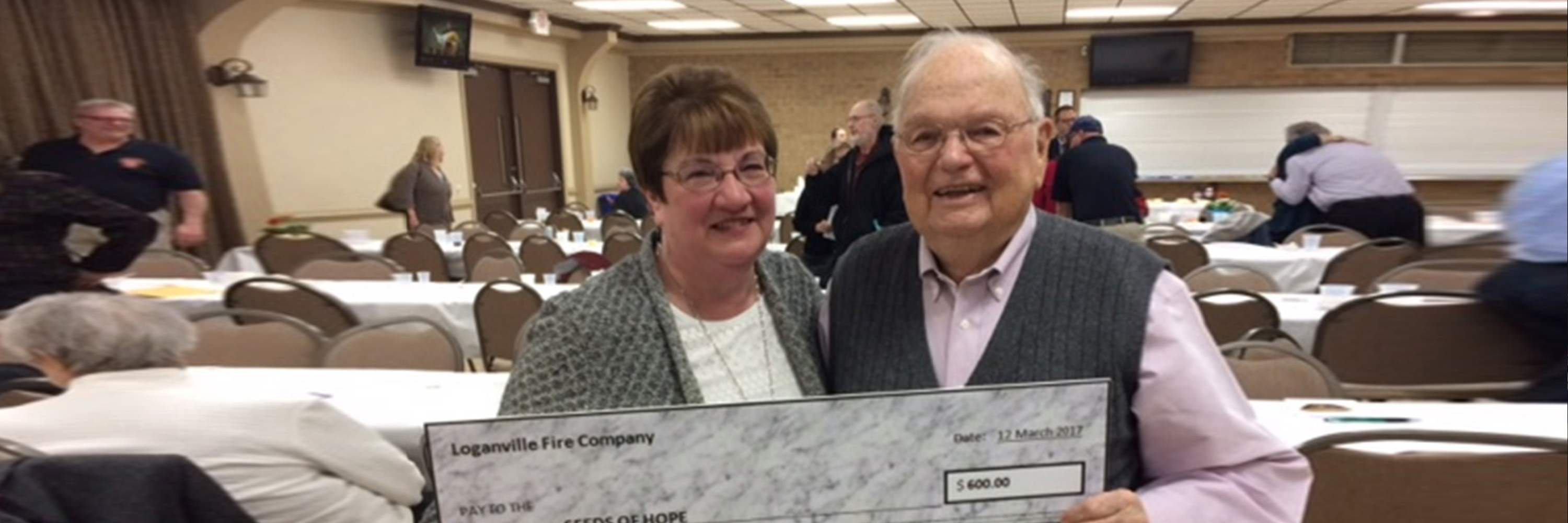
Your financial support allows H.O.P.E. to further its mission of assisting cancer patients and their families.
BE A VOLUNTEER
Volunteers receive guidance and training so they can contribute according & availability.
GET HELP
Our services and programs are available to anyone with a diagnosis of cancer. We are here to help.
Welcome to H.O.P.E.
H.O.P.E. stands for Help for Oncology Problems and Emotional Support

WE'RE HERE TO HELP. FIND OUT WHAT SERVICES & PROGRAMS WE OFFER.
There are moments when words just aren't necessary and a caring hand is all the heart desires. This can be a team of support to fetch the week's groceries or cook meals, a willing individual to coordinate doctor appointments, or maybe just a hand-written note to say hello. The unexpected journey of cancer often brings exhausting emotional challenges and financial burdens. H.O.P.E. helps ease this journey. We invite you to explore our website to learn more about the services, resources, and emotional support that H.O.P.E. provides to those in our community who are affected by cancer.
For Cancer Patients & Families